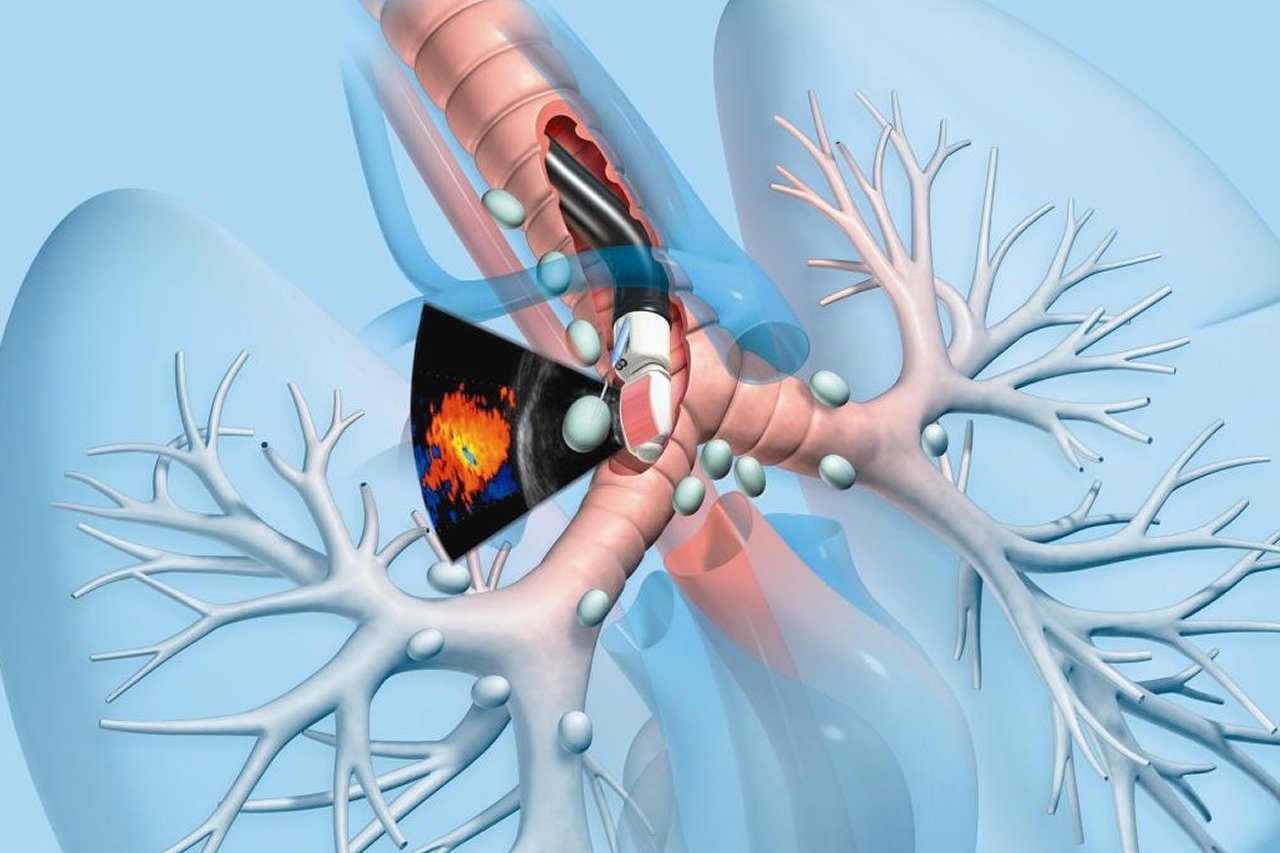
Endobronchial ultrasound (EBUS) is a bronchoscopic technique that uses ultrasound to visualize structures within the airway wall, lung, and mediastinum. Real-time endobronchial ultrasound-guided TBNA (EBUS-TBNA) using the convex probe EBUS allows real-time sampling of mediastinal and hilar lesions. EBUS and guided sampling is gaining popularity and have become a useful and important modality because of their high diagnostic yield and lower risk. There is a potential that EBUS may surpass and replace invasive methods for staging lung cancer and for evaluating mediastinal lymphadenopathy and lesions in the future.
Physicians should have knowledge of mediastinal lymph node stations and sonographic anatomy of the airway wall
1. Staging of non-small cell lung cancer (NSCLC)
EBUS-guided transbronchial needle aspiration (TBNA) has a higher diagnostic yield than conventional TBNA in all lymph node stations except subcarinal lymph nodes in determining the lymph node involvement in NSCLC. It can be combined with an endoscopic ultrasound-guided fine-needle aspiration to a near-complete sampling of mediastinum using a single endobronchial ultrasound bronchoscope.
2. Evaluation of mediastinal adenopathy of unknown etiology, Mediastinal masses, intrapulmonary pulmonary nodules, and endobronchial lesions
EBUS helps to sample and diagnose various mediastinal abnormalities including sarcoidosis, TB, and mediastinal lymphoma. The most common use for EBUS-TBNA in this setting is in patients with bilateral hilar adenopathy where sarcoidosis needs to be distinguished from lymphoma. The value of EBUS-TBNA in obtaining tissue to diagnose benign lesions other than sarcoidosis (eg, tuberculosis, fungal disease) has also been reported
3. Guidance of endobronchial therapy
EBUS provides useful additional information during various interventions like resection of the endobronchial lesion, stricture dilatation, stenting, laser therapy, and argon plasma coagulation.
EBUS is usually performed under procedural sedation and local anesthesia. Local anesthesia on airways is done by nebulizing 1% or 2% lidocaine and spraying lidocaine spray in the posterior pharynx. A 1-2 mL of 1% to 2% lidocaine can be installed through the working channel of the bronchoscope during insertion and procedure if needed.EBUS can also be done under general anesthesia in selected patients if required.
One should not eat or drink at least 6 hrs before the procedure. You may be asked to discontinue blood-thinning medications several days prior to the procedure. A thin tube called a bronchoscope is placed in the mouth. It is difficult to speak once the bronchoscope is in the airways. You will be monitored closely for two to four hours after the test. A chest x-ray will be performed. You must not drive an automobile on the same day. A family member or friend must be available to drive or accompany you home. You may have a mild sore throat, hoarseness, cough, or fever. If the lung is punctured, it can cause an air leak (pneumothorax), which results in lung collapse. If you have increasing chest pain or shortness of breath, or if you cough up more than a few tablespoons of blood, you should contact your doctor. The result of the test may take a few days.
Continuous monitoring of cardiac rhythm, heart rate, respiratory rate, oxyhemoglobin saturation, and blood pressure is usually done after the procedure until the effects of sedation and upper airway anesthesia have been resolved. Eating and drinking can be resumed once the gag reflex returns.
EBUS and EBUS-TBNA are usually safe procedures. No serious complications were found on a systematic review of the effectiveness and safety of CP-EBUS-TBNA of regional lymph nodes. Reported complications are agitation, cough, hypoxia, laryngeal injury, fever, bacteremia, and infection, bleeding, pneumothorax, and broken equipment becoming stuck in the airway. Complications related to upper airway local anesthesia are laryngospasm, laryngeal edema, bronchospasm, methemoglobinemia, and cardiac arrhythmias. Complications attributable to procedural sedation are respiratory depression, cardiovascular instability, vomiting, and aspiration.

